Currance revenue cycle management blends human and digital resources to deliver high-performing work teams, improved data, streamlined processes, and optimized performance increasing revenue.
Revenue cycle
differently

A different approach to revenue cycle management
Currance delivers a performance-driven approach that uses both financial and process metrics, flexible business models, with a blend of technology, support, and intelligence to collect more cash on earned revenue.
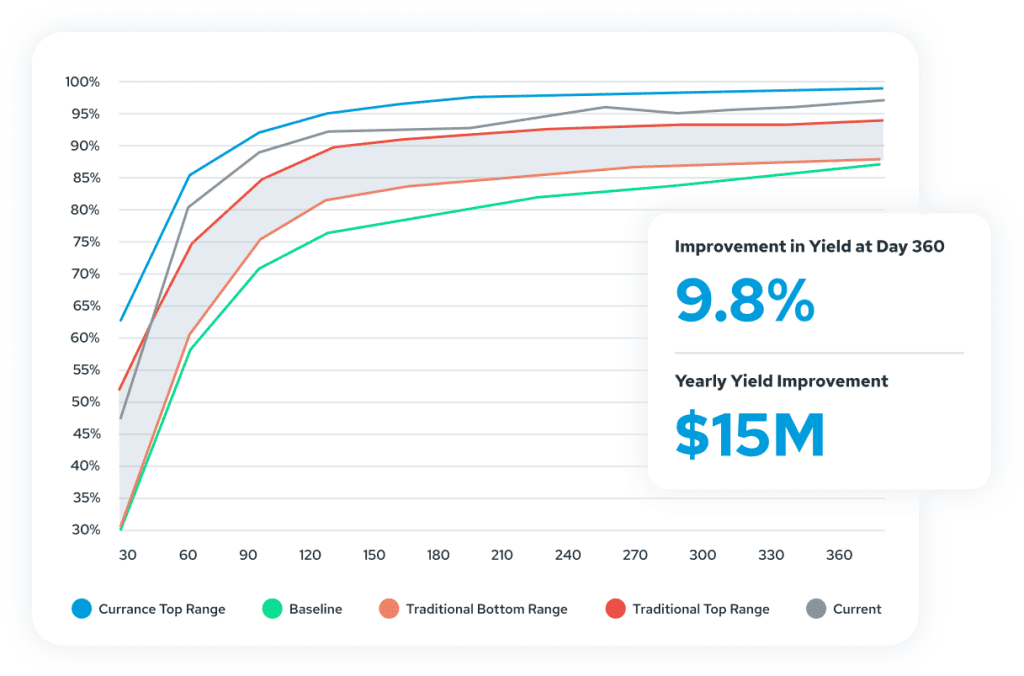
Revenue cycle yield improved up to
6%
Collect more cash
Nonvalue-added work reduced up to
35%
From transactional activities to standard and effective
Account receivables days eliminated up to
25%
Accelerated cash from earned revenue
See how other health systems have improved performance by partnering with Currance.
Let’s talk about how taking a different approach to revenue cycle management delivered an 8-figure revenue improvement for this healthcare system.
Join the Currance crew
